Transurethral resection of bladder tumour (TURBT) at Highgate Hospital
TURBT uses a resectoscope to access and operate on the bladder via the urethra.
What is a bladder tumour?
Abnormal cell growth in the lining of your bladder can lead to the development of benign (non-cancerous) or malignant (cancerous) tumours.
If the tumour is cancerous, it can either be non-invasive or invasive:
- Non-invasive tumours – these tend to stay in the lining of your bladder, which is the most common form of bladder cancer and usually isn't life threatening, but there's a small chance it could develop into an invasive tumour
- Invasive tumours – these are cancers that grow into your bladder wall and can spread to other areas of your body.
What is transurethral resection of bladder tumour (TURBT)?
This procedure involves inserting a thin, tube-like telescope called a resectoscope through the urethra to resect (scrape away) any bladder tumours. Sometimes this tissue is collected and then examined under a microscope to find out what type of tumour you have.
Is TURBT right for me?
If you have a bladder tumour, you may experience blood in your urine (haematuria), a burning sensation when you pass urine, and you may also feel the need to urinate often. Sometimes blood clots can form, which may prevent your bladder from emptying.
To diagnose and ease any symptoms, your consultant may recommend a resection (or scraping) of your bladder.
What are the benefits of TURBT?
Your symptoms should improve. Scraping away a non-invasive bladder tumour should remove it completely and reduce the risk of you developing an invasive cancer.
If you have invasive cancer, a TURBT won't remove the cancer completely, but examining the tissue under a microscope will help your surgeon recommend the best treatment for you.
What happens during TURBT?
TURBT is usually performed under general or spinal anaesthetic. The procedure takes around 30 minutes.
Before the procedure
There are a few things you can do in the lead-up to the operation to make sure everything goes smoothly:
- Let your doctor know about any medication you take and follow their instructions
- If you smoke, stop smoking several weeks before the procedure to reduce your risk of complications – smoking is one of the main reasons why many people have this cancer, so stopping smoking will also lower the chances of new bladder tumours forming
- Try to maintain a healthy weight
- Exercise regularly to help your body prepare for and recover from the operation.
During the procedure
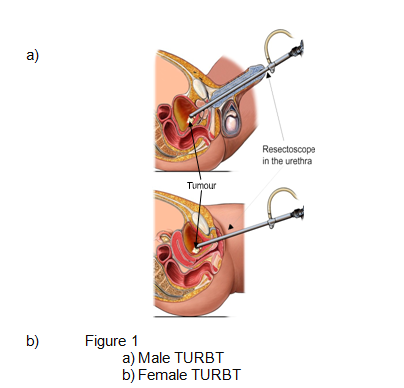
- Once you're under anaesthetic, your consultant will pass the resectoscope into your bladder via your urethra, to examine your bladder lining and locate any abnormal growths
- Any tumours will be scraped and removed from your bladder, and then any exposed or raw areas will be sealed using an electric current – sometimes biopsies (samples of the growth) are taken so they can be analysed in a lab
- After removing the resectoscope, your consultant will place a catheter (tube) in your bladder to help you pass urine easily and wash out your bladder with fluid.
After the procedure
Immediately after your procedure you'll be taken to the recovery room where you'll wake up (if you had general anaesthetic). A nurse will be there to look after you.
Once the effects of the anaesthetic have worn off, you'll be taken to your room. You may be prescribed antibiotics to help prevent infection.
Recovery from TURBT
You’ll usually be in hospital for around 2 days. Most people make a good recovery and return to normal activities within a week or so.
Short-term recovery
You'll be able to leave hospital once you can pass urine on your own after the catheter is removed, which may take 1–2 days.
You won't able to drive, so you'll need someone to take you home when you're able to leave.
Managing your recovery at home
To prevent blood clots, follow the instructions from our healthcare team on medication or special compression stockings.
For the first few days, you may experience a stinging sensation when you pass urine, as well as blood in your urine. This should clear up after a few days.
Here are a few things you can do to make sure you recover well:
- Drink plenty of water to help flush out your bladder
- Avoid any strenuous activity for about a week
- Slowly build up to regular exercise again after the first week.
Driving after TURBT
Don't drive until you can control your vehicle, and always check with your insurance policy and with the healthcare team.
Time off work after TURBT
You should be able to return to work after about 2 weeks.
Follow-up consultations
We'll book you in any follow-up appointments before you leave. If we need to examine any tissue samples, you'll need to come back for the results of these.
Your consultant may suggest additional treatment, depending on the lab analysis. For example, they may recommend a single dose of chemotherapy directly into your bladder through a catheter (intravesical chemotherapy). Even though you may not have an invasive cancer, this kind of chemotherapy can reduce the risk of new growths forming.
Complications of TURBT
As with any surgical procedure, there could be complications, such as:
- pain
- bleeding
- infection
- reaction to anaesthetic
- blood clots (deep vein thrombosis – DVT)
Specific complications of TURBT can include:
- damage to your bladder
- difficulty passing urine
- narrowing of your urethra (urethral strictures).
The healthcare team will do their best to minimise any risks. Make sure you discuss any concerns you have about these complications with your consultant.
17-19 View Road, Highgate, London, N6 4DJ
Ways to pay
Nuffield Health promise
Our prices are all-inclusive. We will equal any comparable price. There are no time limits on your aftercare.
Paying for yourself
There are no hidden costs in our treatment prices. The price you see is the price you pay.
Find out morePersonal medical loan
Spread the cost of your treatment with a 6, 10 or 12 month 0% personal medical loan.
Find out moreMedical insurance
We work with you and your insurance provider to get you the treatment you need quickly
Find out more