Using 3D Printed Titanium Cages for Spinal Surgery
It was a huge relief for Debra Rust when Nuffield Health Leeds Hospital’s consultant orthopaedic spine surgeon, Mr Almas Khan, was able to spot instantly the problem with her spine.

“I had already had an operation on my back five years ago and the symptoms were remarkably similar but this time the MRI scans were not showing anything.
“The pain down my leg was having an enormous impact on my life. I had to stop working as a hairdresser because I could not stand or sit for a long time. Even if I went out to a restaurant I would have to sit and stand mid-meal. It was horrendous.”
This led Debra to think it might be a hip problem, and that’s when she decided to make an appointment at Nuffield Health Leeds Hospital, resulting in two steroid injections to her hip but the pain didn’t dissipate so she was advised to meet to Mr Almas Khan.
“Visiting Mr Khan put my mind at rest. We discussed my history, and he arranged a new MRI and further scans. When he told me had found the problem just above where I had my last operation it was a great relief. I won’t forget hearing the words: “that’s the culprit!” I was so pleased knowing there was an actual problem that could be fixed.

“Even I could see the bulge on the new scan.”
The next steps could have been worrying for Debra
Following her previous surgery at another hospital, she contracted meningitis and sepsis – “it was touch and go” she says.
But that wasn’t going to deter her from a second operation, this time at Nuffield Health Leeds Hospital.

Mr Khan explained that steroid injections would not be effective, and the most reliable course of action was to get rid of the bulging disc by putting a cage in Debra’s back,
Mr Khan explains: “The imaging had shown a narrowing due to a combination of wear and tear leading to some abnormal movement of the bones which, as a result, ended up pressing on the nerve coming down her leg.
“There are a few traditional ways to treat this problem. One of them is to take away the areas of tightness via an operation which involves removing elements of the bone in the area that has narrowed. Normally when we do this procedure, we often must hold the bones in position, so they don’t move any further, that process is called a fusion. The traditional way is to open the area of the spine in question and put screws and rods either side of where we have to remove the bone and put a graft in to join the bones together.”
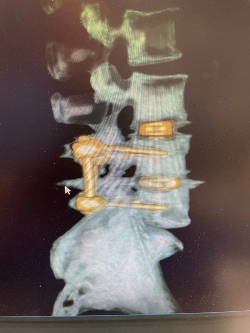
Using innovative technology, a cage would be placed from the side of Debra’s spine instead, to push the bones back up to their original position.
This is known as an indirect decompression. Rather than taking bone away the surgery reconstitutes the shape of the spine.
How does this work? Instead of having the patient on their front and elevating the muscles away from the spine, which means having to cut parts of the muscle and bone that are next to the nerve, a special cage is inserted that works a bit like a wedge between the bones pushing them back into their original position.
The 3D printed construction of the cage means the bones are then able to grow into it eliminating the need for screws or rods or cutting into any of the muscle.
However, because Debra ended up in ICU after her first operation at a different hospital, she wanted to be sure there wasn’t a risk of infection.
“I had an ulcer under my foot and Mr Khan asked one of the foot and ankle consultants to take a look at it. He soon established the reason for its recurrence, in essence it was due to a bent toe. An operation was recommended on my toe and two screws were put in, once that had healed, I had the main operation,” Debra said.
Mr Khan was also keen to ensure any risks were minimised.
“The advantage of going in from the side is that we go don’t have to cut muscles to put the cages in, all we need to do is just separate the muscle fibres. It means people heal a lot more quickly and with less pain and are less likely to get infected because we know that when we go from the back of the spine it can lead to a higher rate of infection compared with entering from the side or the front of the spine, especially when going through an area which has been operated on before.
“It cuts out risks of splitting the muscle with hardly any wound pain afterwards. Of course, there is a little pain from cutting the skin, it’s more of a bruising pain around the muscle.”

The bone only has to grow a few millimetres into the cage to secure it, which takes between six weeks to three months to make the cage solid.
The operation went well, and soon after Debra visited Mr Khan for a further scan.
“I was delighted. It’s been fantastic there’s no pain. It’s also reassuring that he said he will not discharge me for two years to make sure if I have any worries, concerns or pains I can make an appointment.
“Mr Khan was really thorough making me feel at ease. He answered all my questions, and I don’t think I could have asked for more.”
Read more about the Centre for Spinal and Neurosurgery
