Endoscopic sleeve gastroplasty
- Overview
- What is endoscopic sleeve gastroplasty?
- Is endoscopic sleeve gastroplasty right for me?
- What are the benefits of endoscopic sleeve gastroplasty?
- How much weight will you lose?
- How to prepare for endoscopic sleeve gastroplasty
- What happens during endoscopic sleeve gastroplasty?
- How long does the endoscopic sleeve gastroplasty take?
- What happens after endoscopic sleeve gastroplasty?
- Going home after endoscopic sleeve gastroplasty
- Risks and complications
- Find your nearest hospital
- Ways to pay
- Related articles
- Contact us
An endoscopic sleeve gastroplasty (ESG) is a minimally invasive weight loss procedure that reduces the size of the stomach, without any external cuts.
What is endoscopic sleeve gastroplasty?
An endoscopic sleeve gastroplasty (also known as ESG) is a minimally invasive weight loss procedure that reduces the size of the stomach, using an endoscope. This results in significant weight loss by limiting the amount of food you can eat. Since there are no external cuts, an ESG reduces the risk of complications and allows for a quicker recovery compared to other weight-loss surgeries.
Is endoscopic sleeve gastroplasty right for me?
An experienced multidisciplinary team (a mix of health and care professionals) will decide if this procedure is suitable for you and may recommend ESG if:
- You have a BMI between 30 and 50 kg/m²
- You haven't been able to lose weight through diet and exercise
- You are not eligible for, or do not want, traditional bariatric surgery
- You do not have any other medical or psychological conditions that would make you unsuitable for the procedure
What are the benefits of endoscopic sleeve gastroplasty?
For people with obesity, losing weight through ESG can help reduce the risk of weight-related health issues, including:
- Heart disease
- Liver disease
- Diabetes
- High cholesterol
- High blood pressure
- Joint pain and osteoporosis
- Sleep problems
Other benefits of endoscopic sleeve gastroplasty include:
- Lower risk of complications: ESG has a reduced risk of complications compared to traditional gastric sleeve surgery.
- Shorter recovery time: Patients can typically expect to return to work within a few days to a week, rather than the usual 8-week recovery for traditional recovery.
- Organ-preserving: Unlike traditional gastric sleeve surgery, which involves surgically removing a portion of the stomach, ESG reduces the stomach's size using internal sutures. This method creates a narrow, sleeve-like shape without removing any part of the stomach, thus preserving the organ's structure and function.
How much weight will you lose?
Combined with healthier lifestyle changes, endoscopic sleeve gastroplasty can help you lose up to 20% of your total weight1.
How to prepare for endoscopic sleeve gastroplasty
Your multidisciplinary team will tell you how to prepare for your endoscopic sleeve gastroplasty. They will:
- Review your medical history and current medications: You may need tests such as blood work, scans, or heart recordings to ensure you are safe to undergo general anaesthesia.
- Advise you on a pre-procedure diet: You may need to follow a low-calorie diet for a few days before the operation. This diet helps reduce the fat content in your liver, making the operation safer.
- Provide fasting instructions: You will receive specific instructions on when to start fasting before your procedure.
By following the guidelines and any additional instructions from your multidisciplinary team, you can ensure you are well-prepared for your endoscopic sleeve gastroplasty.
What happens during endoscopic sleeve gastroplasty?
You will be given general anaesthesia, putting you in a sleep-like state. Your medical team will monitor your vital signs throughout the procedure.
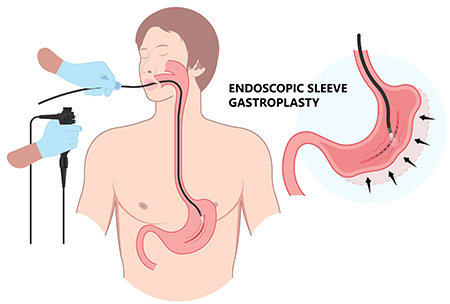
Your surgeon will insert an endoscope (a long, flexible tube with a light, camera and suturing device) through your mouth, down your oesophagus and into your stomach. They will release gas into your stomach to expand it.
Using the camera and suturing device on the endoscope, your surgeon will place several stitches inside your stomach to create a narrow pouch or sleeve. These stitches are safe and will not dissolve, but they can be removed if the procedure needs to be reversed.
The size of your stomach will be reduced by about 70%, meaning you will feel fuller longer, absorb fewer calories, and lose weight.
How long does the endoscopic sleeve gastroplasty take?
The procedure takes approximately 60 to 90 minutes.
What happens after endoscopic sleeve gastroplasty?
After the procedure, you will be taken to the recovery area and monitored closely before being transferred back to the ward. You may need to stay in the hospital for one or two nights following your procedure.
You may have an IV in the back of your hand to give you fluids. This will be removed once you are hydrated and able to drink enough fluids on your own. You may also have a catheter (a tube placed into your bladder) that will be removed at the end of your procedure.
It is normal to experience some pain, nausea, and vomiting after endoscopic sleeve gastroplasty. You will be given pain relief and anti-nausea medication as needed.
You will start with a liquid-only diet for the first two weeks after your procedure to give the stitches in your stomach time to heal. You can then progress to soft foods and eventually to solid foods. Your multidisciplinary team will provide you with detailed instructions on your diet.
Going home after endoscopic sleeve gastroplasty
You should have someone to take you home after the procedure. You will be given medication to take home, including blood thinner injections. You will be shown how to administer these injections.
Once you are home, it is important to rest, but try to move around and avoid staying in bed all day. Drink plenty of fluids and follow the diet your doctor has provided.
You can return to work when you feel able to resume normal activities. This may be a few weeks after your procedure, but it could be longer depending on the type of job you do. You should not lift heavy objects for 8 weeks after the procedure.
Follow-up appointments after endoscopic sleeve gastroplasty
You will need to regularly see your doctor and dietitian after the procedure to make sure you are recovering and adapting well.
Risks and complications
Your doctor will discuss all the risks and possible complications before your procedure. You may experience some complications, including:
- Sore throat
- Pain
- Nausea
- Vomiting
- Abdominal pain and/or bloating
- Infection
- Stitches not healing properly
All procedures that are carried out with an endoscope carry some degree of risk, including:
- Approximately 1 in 5000 patients are at risk of perforation of the stomach
- Approximately 1 in 5000 patients are at risk of perforation of the oesophagus
- Approximately 1 in 500 patients are at risk of excessive bleeding during the procedure
If you have any concerns, please speak to your doctor.
Source:
1 Mayo Clinic
Parkside
020 8971 800053 Parkside, Wimbledon, London, SW19 5NX
Tunbridge Wells
01892 531 111Kingswood Road, Tunbridge Wells, TN2 4UL
Ways to pay
Nuffield Health promise
Our prices are all-inclusive. We will equal any comparable price. There are no time limits on your aftercare.
Paying for yourself
There are no hidden costs in our treatment prices. The price you see is the price you pay.
Find out morePersonal medical loan
Spread the cost of your treatment with a 6, 10 or 12 month 0% personal medical loan.
Find out moreMedical insurance
We work with you and your insurance provider to get you the treatment you need quickly
Find out moreAsk a question about this treatment
Fill in the form below and we'll get back to you within one working day.
Thank you
A member of the team will respond to you soon.

