Bone density scanning for osteoporosis explained
- Overview
- Full article
- Related articles
Osteoporosis is commonly thought to be a disease that only affects post-menopausal women. But from the age of 40, our ability to retain calcium in our bones is diminished - leading to a loss of bone mass and strength. Dual-energy X-ray Absorptiometry (DXA) scanning, also known as Bone Mineral Densitometry (BMD), can calculate your bone density in a matter of minutes, using very low dose radiation (less than a common chest x-ray). Your bone density 'T score' can fall into three ranges: normal, osteopenic (the range between normal and osteoporotic), or osteoporotic. Knowing your T score can help your GP to prescribe medicine and suggest dietary and lifestyle changes that may improve your bone density and lower your risk of breaking a bone.
The patient

Name: Sally Wood
Age: 55
Risk factors: Post-menopausal, previous history of eating disorders, back pain. Click for more info on risk factors.
The expert

Name: Chris Tomlinson
Position: Lead Bone Densitometry Radiographer at Nuffield Health York Hospital
Year of qualification: 1975 (40 years' experience)
The DXA scan
Step 1
After being correctly identified Sally is asked to change into a gown to ensure she's not wearing any metal near the areas where she'll be scanned. Metal can interfere with the accuracy of the scan. It's not necessary for her to take all her clothes off as long as she doesn't wear anything bulky. She then sits down with Chris and answers a questionnaire before being weighed and measured.
Step 2
Chris creates a profile and inputs Sally's weight, height, ethnicity, age and gender. The information obtained in the scans will be compared against an international database to calculate the results.
Step 3
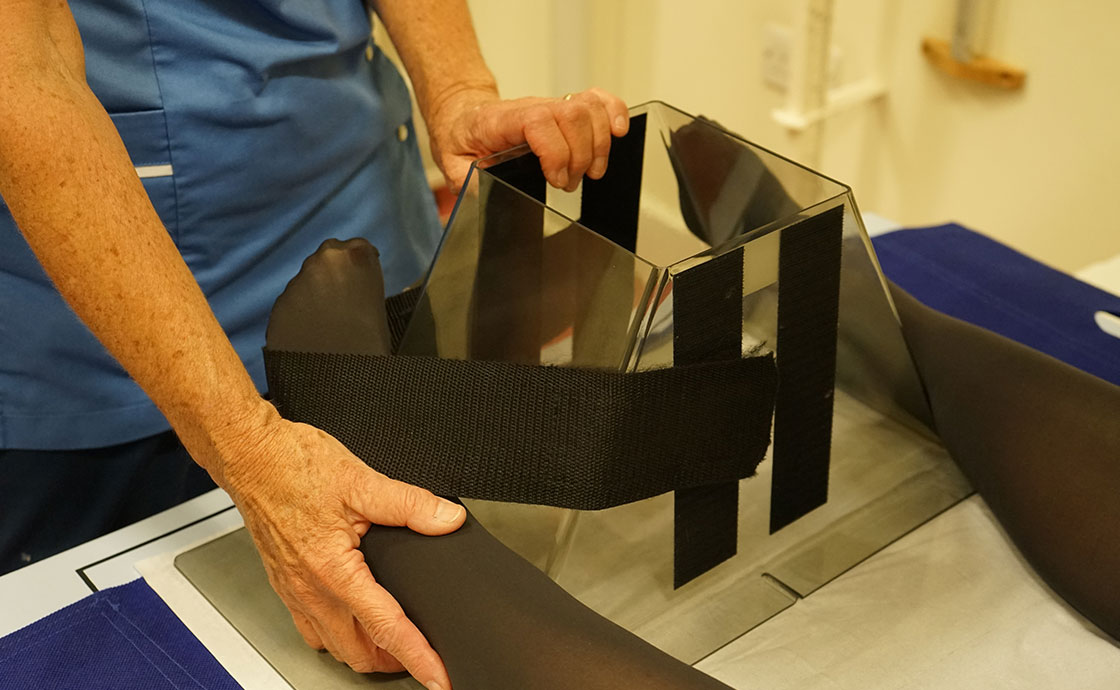
Chris helps Sally to position herself on the bed. Two areas of her body will need to be scanned, her hip and lumbar spine (lower back). These bones are large and help to give an accurate reading. To more clearly scan the hip, Chris straps Sally's foot to a block at the end of the bed, ensuring she holds her leg at the optimal angle for scanning. Chris then positions the aiming light target over the hip.
Step 4
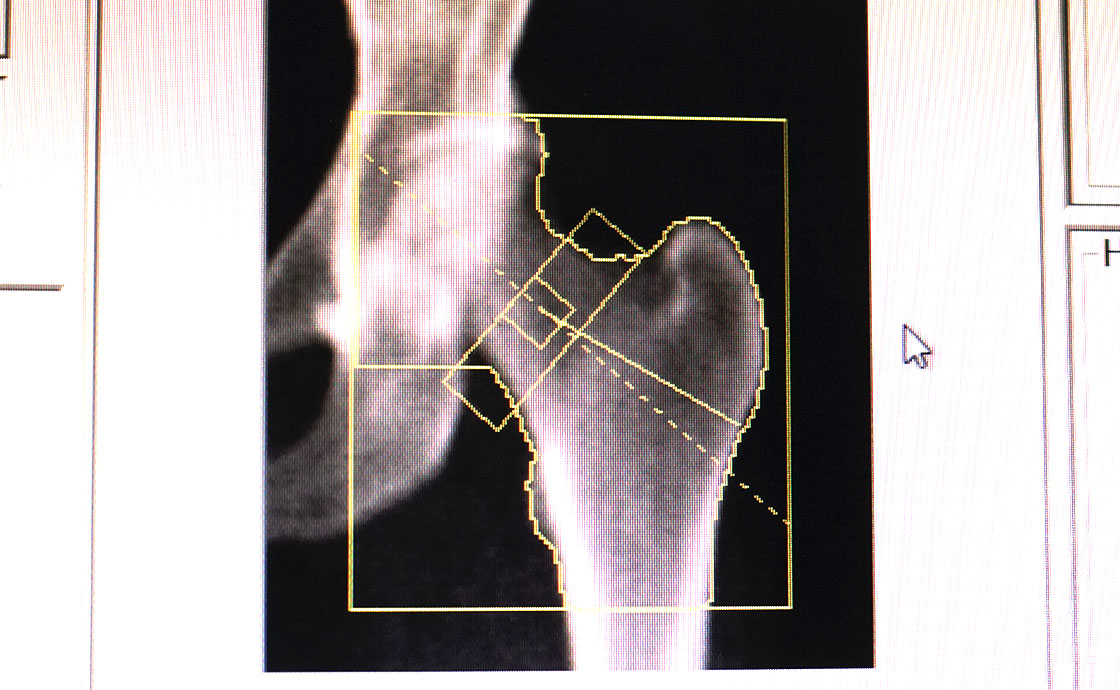
Chris moves back to her computer to start the scan. The radiation levels are so low that she doesn't need to sit behind a screen as long as she is a set distance away from the beam. An image of Sally's hip bone appears immediately on the monitor. Chris then analyses the image to ensure the optimum result.
Step 5
Steps 3 and 4 are repeated but this time Sally's spine is targeted. To get a clear scan, Sally's legs are positioned on a block to reduce the curvature of her spine. Sally had an operation to fuse her lower spine some years ago, the metal implant is visible in her scan. Chris makes sure none of the metal is included in Sally's results.
Step 6
Because Sally was referred with back pain, and on the request of her Consultant, Chris conducts an additional test called an Inter Vertebral Analysis (IVA). This will look for undiagnosed fractures in the spine that could also indicate osteoporosis.

The results
Sally's results are compared to a range of young healthy adults with average bone density. The difference between Sally's results and the average is expressed as a standard deviation (SD) and given as a T score.
- T score between 0 and -1 is considered normal
- T score between -1.1 and -2.4 is termed osteopenia
- T score below -2.5 is classed as osteoporosis.
These results are reported by a Consultant radiologist and can be forwarded to Sally's GP or Consultant straight away. She'll be able to discuss her results within a few days at her next appointment.
Diagnosis
Sally's T score is in the osteopenic range. That means her bones have a lower density than normal but she's not quite osteoporotic. The good news is Sally can now take steps to delay or even prevent osteoporosis from taking hold.
A Consultant may recommend adjusting her diet to boost her intake of calcium, more weight-bearing exercises such as walking, and to make sure she's getting enough vitamin D by spending time outside in the sunshine. If future tests indicate Sally is moving closer to the osteoporotic range, then she might be prescribed medicine that helps her bones to retain calcium. These simple steps might be enough to make sure Sally never develops osteoporosis and doesn't unexpectedly break or fracture a bone in a minor fall.
For osteoporosis support and information visit the National Osteoporosis Society.
Last updated Friday 14 December 2018
First published on Monday 19 October 2015