Inside the pathology lab | What happens to my blood?
- Overview
- Full article
- Related articles
As a pathology manager I lead a team of biomedical scientists who's job it is to analyse and interpret blood and fluid samples we get from the hospital. Without running diagnostics, GP's and Consultants would be left to play a guessing game, relying on symptoms alone to diagnose conditions. With the help of technology, we can pin point tiny substances in your blood, so you can be prescribed the right treatment.
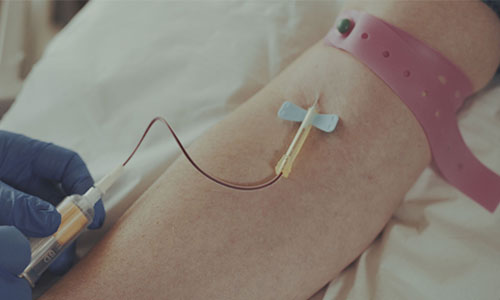
Step 1
Before we can test your blood, we have to take it. It's not unusual to be a bit squeamish about this. But the act of taking blood is very safe and most patients find it painless. Using a hypodermic needle, a phlebotomist will take one or more tubes of blood using a vacuum system. This helps us to get several samples to run multiple tests with just one prick of the needle. Find out more about the phlebotomy procedure.

Once the blood sample is taken, it's labelled before being collected and transferred to the laboratory. As the samples are passed over, the details are checked and recorded on our computerised lab system which keeps track of them throughout their time in the lab.
Step 2
Depending on the reason for your blood test, the samples are split into two groups.
Group 1
If we want to look at general markers of health like the number of red and white cells, then the samples are placed in an automated Full Blood Count (FBC) Analyser. The machine takes up a quantity of the blood and holds it in a thin glass tube. Beams of light are fired through the tube, counting cells and noting their type based on their interaction with the light. It also measures haemoglobin levels, the protein in red blood cells that carries oxygen around the body. The computerised results are extremely accurate and obtainable within minutes of running the test, giving us a reliable snapshot of overall health.
Group 2
The second group requires more intervention. Markers of more specific conditions tend to be found within the blood serum. A Centrifuge spins the blood samples at 3000 RPM for five minutes, forcing the cells to the bottom of the sample and leaving the serum at the top. This allows the contents of the serum to be analysed without interference from the cells.
Step 3
The serum samples are then moved to the chemistry section of the lab. We have two machines: the Cobas c 311 clinical chemistry analyser and e 411 immunoanalyser. The c 311 looks for substances found in larger quantities in the blood that impact body function, especially the liver or kidneys. It can also run diagnostics on metabolism.
The e 411 is able to detect substances at much lower quantities and is able to check for literally thousands of disease indicators, including cancer markers. The machine can also measure hormone levels, playing a vital part in fertility diagnostics for assisted conception services.
Both machines work by producing a coloured reaction by exposing the sample to different chemicals. The colours can't be seen with the naked eye but a sensitive light beam can very accurately detect tiny amounts of substances in the blood, and use the information to diagnose diseases and other health issues.
Step 4
The technology used in the lab helps to automate extremely delicate processes that produce very reliable results. However, the results are meaningless unless the machines are operated by highly skilled professionals who can critically analyse and interpret the results for themselves.
All pathology results need sign off from a biomedical scientist before they can be authorised. It's all part of our fully accredited process that governs documentation, management and quality control.
Step 5
Once authorised, the results can be printed and sent to the health professional who requested them. The results are also available via a web-based system called Cyberlab. This allows the requester to view the results any time, any where.
Step 6
With the results in hand, your GP or Consultant may now have new and vital information about what's going on inside your body. A solid, evidence-based diagnosis is hugely important in receiving effective treatment.
Last updated Monday 2 December 2019
First published on Wednesday 9 December 2015