Hip replacement at Shrewsbury Hospital
This is a procedure to remove your damaged hip joint and replace it with an artificial joint.
What is a hip replacement?
It’s used to treat hip pain, most commonly hip osteoarthritis, which is gradual wear and tear of the joint.
During the procedure, the damaged joint is removed and replaced with an artificial ball and socket joint (a prosthesis). There are many different types of hip replacement and your surgeon will recommend the one that’s best for you.
Is a hip replacement right for me?
Your consultant may recommend a hip replacement if:
- your hip pain is so severe that you can’t sleep at night
- you’re having trouble walking
- you’ve tried alternative treatments and they haven’t helped
It’s usually only offered if:
- you’re over 60
- you have a weak thigh bone
What are the benefits of a hip replacement?
You should have much less pain and be able to walk more around easily.
How long do the benefits last?
Hip replacements can wear out over time, depending on your body weight and how active you are. Most people’s hip replacements last around 15–20 years. After that time, you’ll need a hip revision.
What happens during a hip replacement?
Hip replacements usually take around 1–1.5 hours. It’s usually done under spinal anaesthetic to numb the lower half of your body, and you’ll be given a sedative to relax you. Another option is general anaesthetic, which sends you to sleep. Your anaesthetist will discuss your options with you.
Before the procedure
There are a few things you can do in the lead up to the procedure to make sure everything goes as smoothly as possible:
- Let your doctor know about any medication you take and follow their instructions
- If you smoke, stop smoking several weeks before the operation
- Try to maintain a healthy weight
- Exercise regularly
- Try to have a bath or shower either the day before or on the day of the operation
During the procedure
- Once you’re under anaesthetic, your surgeon will make a cut in the side of your hip and remove the damaged ball and socket joint
- Then they’ll insert an artificial joint – this will either be fixed to the bone with acrylic cement, or have a special coating that bonds directly to the bone
- Finally, they’ll close the skin with stitches, staples or surgical tape.
After the procedure
You’ll be taken to the recovery room where you’ll come around. A nurse will be there to look after you. You’ll have a large dressing covering your wound and you may have a small tube coming out of it to drain away any excess fluid.
You may also have a drip (infusion) going into your arm to keep you hydrated and give you pain relief. The nurse will check your wound, blood pressure and pulse, and when you’re ready, they’ll take you to your room.
Other types of hip replacement
Minimally invasive hip replacement
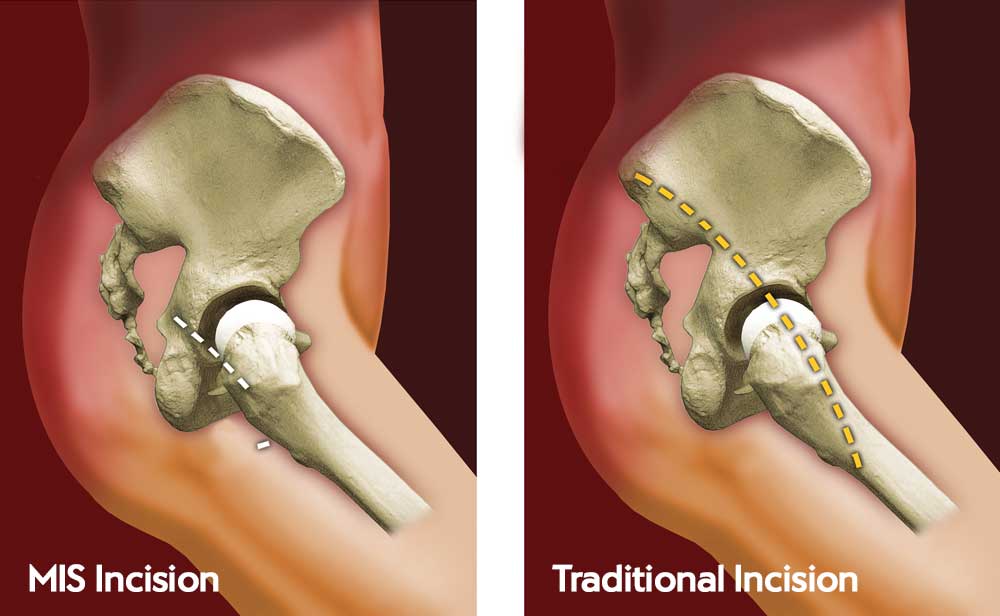
This type of surgery is just as safe and effective as traditional hip surgery, but with quicker recovery times.
In comparison to traditional hip surgery, minimally invasive replacement hip surgery reduces how deep the surgeon creates an incision as rather than cut muscles to gain access to the hip joint, the soft-tissue is simply moved aside, which reduces trauma to the soft-tissue around the hip.
The prosthetics implants are fitted through the small window created between two muscles at the top of the hip. Some of the implants are aligned and impacted with an instrument inserted through an additional keyhole incision lower down the leg.
Bi-lateral hip replacement
Sometimes a patient will have degenerative problems in both of their hips. In these cases, a consultant could consider replacing both hips at the same time, called a bi-lateral replacement.
This would mean only one operation compared to two separate ones, meaning less recovery time overall however it does mean that the surgery would take around four hours compared to two for a single replacement.
Candidates for a bi-lateral hip replacement tend to be younger as the rehabilitation needed after surgery can often be quite rigorous.
Robotic hip replacement
This type of replacement uses the MAKO™ robotic-arm assisted technology to improve the accuracy and precision of the procedure. In the weeks before your operation, the robotic arm processes the information taken from a 3D CT scan of your body. Your consultant then plans the operation to within fractions of a millimetre with the help of the robotic-arm assisted technology, which allows for dynamic joint balancing, more precise implants and more comfortable implants.
During the operation your consultant is always in control, but the robotic-arm assisted technology allows the consultant to perform the joint replacement with pinpoint accuracy. The consultant uses the technology as an extension of his or herself, guiding surgical tools to the correct position. The robotic-arm assisted technology does not perform the surgery on its own.
Higher accuracy means the replacement fits as well as it possibly can and ensures the joint functions as normally as possible after surgery. It's been shown to result in a shorter hospital stay, quicker recovery and higher satisfaction. There's also strong evidence of decreased pain and fewer complications following surgery.
Recovery
Following your operation you’ll be able to go home when your pain is under control, you can get about safely and any care you may need has been arranged.
It may take up to 6 weeks to recover from the operation. It can take up to 12 months before you are back to normal activities.
Short-term recovery
When you’re back in your room, the nurse will keep checking on you to make sure you’re recovering well. Once the anaesthetic has worn off, you’ll be able to have something to eat and drink and start moving your legs.
While you’re in bed, you may have help with the circulation in your legs to prevent blood clots. This can include:
- Wearing boots that are inflated with air for the first 2 days
- Wearing support stockings, which you should leave on for 4–6 weeks
- Daily injections or tablets, which you may have for up to 6 weeks
Walking around again
We understand you may be anxious about getting up for the first time, but we’ll be there to help you whenever you’re ready.
- Day of surgery: A physiotherapist will give you some exercises to do while you’re in bed to help your new hip joint move and strengthen the muscles around it
- Day after surgery: You’ll have an X-ray to check the position of your new hip. The physiotherapist will help you get out of bed and take your first steps – you may need to use a frame to start with. The nurse will then help you walk around until you can do this yourself. You should repeat your exercises hourly
- Second and third day after surgery: A physiotherapist will give you some tips for getting on and off the bed, chair and toilet, as well as washing and dressing. The physiotherapist will help you transfer to crutches or a walking stick, before giving you some more exercises to increase your movement
You’ll be able to go home as soon as you can walk up and down stairs safely and the healthcare team are happy with your recovery.
You won’t be able to drive, so you’ll need someone to come and take you home.
Managing your recovery at home
You may feel quite tired when you get home, so get plenty of rest. Then it’s important to slowly increase your activity.
Here are a few things you can do to strengthen your hip, avoid damaging it and help your wound heal:
- Continue the exercises the physiotherapist showed you 3 or 4 times a day for 6 weeks
- Try low-impact exercises like walking and gradually increase how far you walk
- If moving around is uncomfortable, take any painkillers we’ve prescribed until you’re pain free
- Don’t lift anything heavy or do any strenuous exercise
- Avoid bending your hip beyond 90 degrees
- Avoid rolling your leg towards the other leg or crossing your legs
- Avoid twisting on your hip when standing
- Keep using your crutches or walking stick for as long as you feel you need to
- Shower instead of taking a bath
Call the healthcare team if you have any questions or concerns about anything.
Driving after a hip replacement
It will be around 6 weeks until you're able to drive again, however it could take less or more time depending on the individual. Your doctor will be able to advise as to when you'll be ready, but don’t drive until you’re confident you can control your vehicle, and always check with your insurance company and your doctor.
Time off work
Check with your doctor before going back to work, but as a rough guide, if your job is:
- Sedentary (e.g. desk work) – you’ll be able to return to work after around 4 or 6 weeks
- Mixed-labour (e.g. teaching) – you can return after around 3 months
- Manual labour (e.g. construction) – you should wait around 6 months before you return
Follow-up appointments
You’ll need to come back for a check-up after around 6–12 weeks. We’ll arrange this with you before you leave the hospital.
Risks
Complications are rare but possible. Rest assured that your consultant will weigh up the risks and advantages with you when deciding if they recommend surgery. Your consultant will also discuss any additional risks that apply to your situation at your initial consultation.
Complications of hip replacement are rare, but you could experience:
- split in the femur
- nerve damage around the hip
- damage to the blood vessels around the hip
- infection in the hip
- loosening of the replacement
- bone forming in muscles around the replacement
- dislocation
- leg length difference.
Alternative treatment options
Most hip pain problems don’t usually require surgery and can be eased through non-invasive measures such as painkillers, using a walking stick, physiotherapy and joint injections.
If you’re under 60 and have a healthy thigh bone, your consultant will recommend hip resurfacing. This operation involves removing the surfaces of the ball and socket of the hip joint and replacing them with ceramic covers – so more of the bone is retained.
Hip replacement consultants at Shrewsbury Hospital
Longden Road, Shrewsbury, SY3 9DP
Guide price
| Initial consultation | from £140 | |
|---|---|---|
| Diagnostics | If needed to determine treatment plan | |
| Treatment | £16,830 | |
| Pre-assessment | Included | |
| Main treatment | Included | |
| Post-discharge care | Included | |
| Pre-assessment, Main treatment and Post-discharge care | £16,830 | |
| Guide price | £16,970 | |
The guide price
stated above is an approximation of the cost of treatment only. The final price
may vary according to Consultant fees, prosthesis or drugs used and any
pre-existing medical conditions which may alter your care pathway.
You will be given a fixed all-inclusive price for treatment following
your initial consultation with a Consultant.
Ways to pay
Nuffield Health promise
Our prices are all-inclusive. We will equal any comparable price. There are no time limits on your aftercare.
Paying for yourself
There are no hidden costs in our treatment prices. The price you see is the price you pay.
Find out morePersonal medical loan
Spread the cost of your treatment with a 6, 10 or 12 month 0% personal medical loan.
Find out moreMedical insurance
We work with you and your insurance provider to get you the treatment you need quickly
Find out moreAsk a question about this treatment
Fill in the form below and we'll get back to you within one working day. If it's urgent, you can call us on 0300 123 6200.
Thank you
A member of the team will respond to you soon.



